If you’re suffering from gum disease, you might have questions about whether composite bonding is a viable treatment option for issues like tooth decay, cavities, or problems with the tooth root. It’s natural to wonder about the feasibility and safety of undergoing composite bonding when facing periodontal challenges.
This comprehensive guide is here to shed light on the possibilities of using composite bonding to treat gum disease while addressing common concerns. We’ll help you explore the procedure, so you’ll know exactly what to expect and whether it’s the right option for you, making sure you have everything you need to make an informed decision.
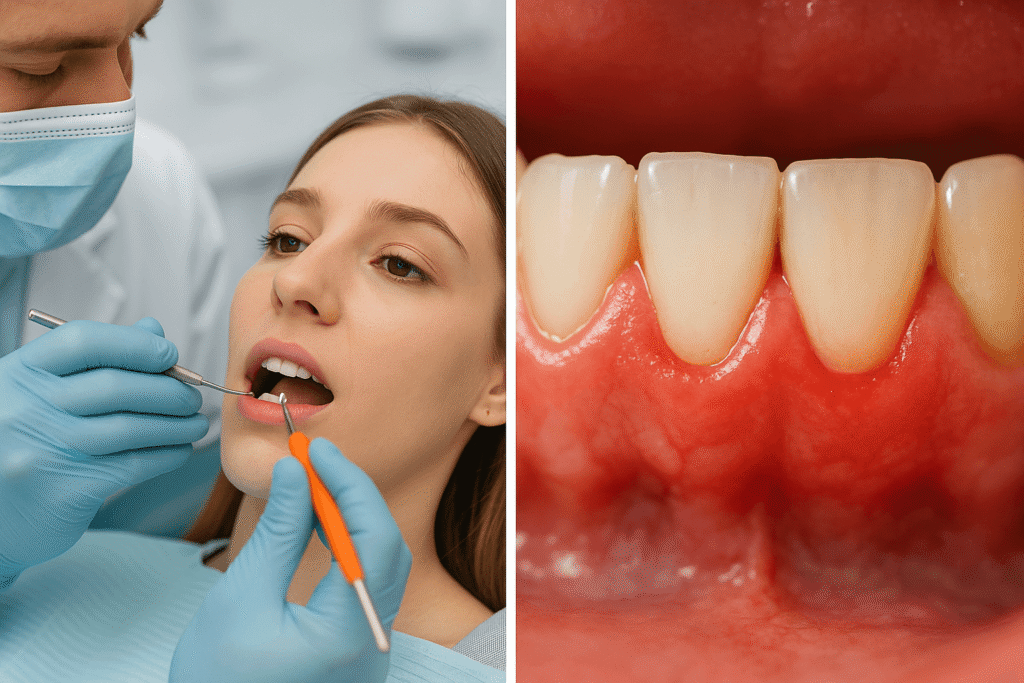
What is Gum Disease and Periodontitis?
Gum disease (or periodontitis) is a serious oral health condition that begins with gingivitis, where bacteria and plaque build up along the gumline, causing redness, swelling, and bleeding. If left untreated, it can progress into more severe periodontal disease, affecting not just the gums, but also the surrounding tissues that support the teeth. Inflammation and infection can lead to gum recession, pockets around the teeth, and persistent bad breath. In advanced cases, tooth mobility and even tooth loss can occur.
The primary cause of gum disease is poor oral hygiene, but there are other factors that can contribute to its development and progression:
-
Plaque buildup, a sticky film of bacteria, accumulating on the teeth
-
Smoking
-
Genetic predisposition
-
Hormonal changes
-
Certain medications
-
Systemic diseases
Regular dental check-ups and good oral hygiene practices are essential for managing and preventing the advancement of gum disease, helping to maintain healthy gums and teeth.
What is Composite Bonding and How Does It Work?
Composite bonding is a cosmetic dental procedure that helps enhance the appearance of your teeth. The process involves applying a tooth-colored resin material to repair damage, close gaps, and reshape your teeth for a more uniform and natural look. Whether you’re trying to improve your smile or correct imperfections, this procedure is a quick and effective way to achieve a more seamless and beautiful smile, even if you’re dealing with gum disease or severe gum recession.
The resin used in composite bonding is made from a mix of plastic and fine glass particles that mimic the natural appearance of tooth enamel. It’s soft and malleable when first applied, allowing the dentist to sculpt and shape it to your desired form. Once shaped, a special curing light is used to harden the material, making it polished and durable. This treatment is especially beneficial for those with periodontal disease, as it can help restore the appearance of your mouth while maintaining a natural look.
Composite Bonding and Gum Disease: What You Need to Know
When it comes to gum disease, the possibility of using composite bonding really depends on the severity of the condition. For those with mild gingivitis, composite bonding might be a viable option, especially if it’s paired with proper dental care. Professional dental cleanings and improved oral hygiene practices can help manage and even eliminate gingivitis, making the procedure safer and more effective. Your dentist will assess the circumstances and determine if composite bonding is a good fit for your needs.
However, if you’re dealing with more advanced periodontitis, it’s crucial to get the gum disease under control first. Issues like gum recession, bone loss, and tooth mobility can complicate the application of cosmetic dental procedures like composite bonding. In these cases, addressing the underlying gum disease through lifestyle changes and professional treatments is key before considering cosmetic options like composite bonding.
Is It Possible to Use Dental Bonding with Gum Disease?
If you have gum disease, it’s important to address the issue before considering dental bonding. Gum disease causes inflammation and infection in the gums, and if untreated, it can lead to further damage.
A dentist will need to treat the gum disease first and assess the severity of gum recession before moving forward with any cosmetic procedures like dental bonding. The right approach will depend on how much damage has occurred and whether it’s appropriate to proceed with the bonding treatment.
The Importance of a Dentist in Composite Bonding Treatment
When considering composite bonding for gum disease, it’s essential to consult a qualified dentist. They’ll assess the condition of your gums and teeth, possibly using X-rays to get a clear picture. Based on this, your dentist can develop a treatment plan that’s suitable for your specific needs. Whether it’s addressing gum disease or ensuring the bonding procedure works well with your gums and teeth, a professional evaluation is key to making sure everything goes smoothly and effectively.
Steps to Addressing Gum Disease Before Considering Composite Bonding
If you’re considering composite bonding and have gum disease, taking steps to manage the condition can increase the likelihood of being a good candidate for the procedure. Here’s what you can do:
-
Regular dental check-ups with your dentist are essential to stay on top of your oral health. These appointments help remove plaque and tartar buildup, reducing the risk of further gum disease.
-
Follow a good oral hygiene routine by brushing twice a day, flossing, and using an antiseptic mouthwash to keep your gums and teeth healthy.
-
Lifestyle changes like quitting smoking, which is a significant risk factor for gum disease, can make a big difference in managing the condition.
-
Managing underlying health conditions like diabetes can also help reduce your susceptibility to gum disease.
-
Maintaining a balanced diet rich in fruits and vegetables supports healthy gums and overall oral health.
Taking these steps can help address gum disease and prepare you for a smoother experience with composite bonding.
How to Care for Your Teeth After Composite Bonding
Taking good care of your dental bonding after the procedure can help prolong the lifespan of the bonding material. Here are some simple aftercare tips to keep in mind:
-
Avoid hard or sticky foods for a few days after the tooth bonding procedure to give the bonding time to set properly.
-
Make sure to brush and floss your teeth regularly, especially around the bonded area, to prevent plaque buildup.
-
Schedule regular checkups with your dentist to monitor the condition of your bonded teeth and ensure everything is holding up well.
-
Keep up with your oral hygiene to maintain the strength of the bonding material and the health of your teeth, especially if you have receding gums.
Taking these steps will help keep your bonding material in great condition for as long as possible, so you can enjoy your improved smile!
How Can Dental Bonding Help with Gum Recession?
Dental bonding can be an effective solution for covering the gaps caused by gum recession. As your gums recede, they can expose the tooth’s root, creating unsightly gaps between your teeth. The bonding material can help fill these gaps, giving you a more even appearance. It can also serve as a barrier against tooth sensitivity, especially when eating hot or cold foods and drinks, reducing sensitivity and providing relief.
Advantages and Disadvantages of Dental Bonding for Receding Gums
Advantages
-
Dental bonding uses composite resins, which are tooth-coloured materials that can be applied to the affected area of your teeth quickly and painlessly by a dentist. The resin is shaped to match the surrounding teeth and hardened with a special light, providing a smooth, natural finish.
-
This procedure is often completed in just one visit, making it a convenient solution for those with severe gum recession.
-
Dental bonding can fill in gaps caused by receding gums, giving your smile a fuller and more even appearance.
-
It’s also a less expensive option compared to other gum recession treatments like gum grafting, making it a good alternative for those concerned about cost.
Disadvantages
-
While composite bonding has many advantages, it also comes with some disadvantages. The bonding material may not last as long as other treatments, such as veneers or crowns, with an average longevity of about 3-10 years before needing to be replaced.
-
Some people may experience allergic reactions to the resins used in the bonding procedures.
-
In severe cases of gum recession, such as with deep pockets around the teeth, gum grafting might still be necessary.
-
The resin material can stain or discolour over time, which can be problematic for those who smoke or frequently consume foods and beverages like coffee or red wine that are known to cause staining.
How Much Does Composite Bonding Cost for Patients with Gum Disease?
The cost of composite bonding can vary depending on factors like location, dentist experience, the number of teeth being treated, and the complexity of the case. On average, patients can expect to pay between $300-$600 per tooth. This is generally less expensive than other treatments such as dental implants or gum grafting, making it a more budget-friendly option for patients dealing with gum disease.
However, the cost might differ based on the dental practice and the care you receive. Some practices offer competitive rates while ensuring exceptional care, cutting-edge techniques, and personalized attention to ensure the best results for patients with gum disease.
Conclusion: Is Composite Bonding a Viable Treatment for Gum Disease?
When dealing with gum disease, composite bonding can be a viable treatment option for receding gums, especially in minor cases or with mild periodontal disease. It offers many advantages, such as being a non-invasive and affordable solution to improve your smile by repairing gum recession and covering gaps. Dental bonding can be compared to other options like veneers, and while it is an effective solution for many, it also has its limitations.
For more severe cases, including bone loss or deep pockets due to advanced periodontitis, composite bonding may not be the best option. It’s essential to consult with a dentist or specialist to weigh the pros and cons, determine the right treatment plan, and address your specific needs. Professional advice, good oral hygiene practices, and regular dental check-ups are key to maintaining long-term oral health while keeping your treatment cost-effective and time-efficient.



